

The researchers concluded that the SARS-CoV-2 spike protein might damage the heart via TLR4 inflammatory pathways, independently of ACE2. This, they noted, means that mRNA vaccines are unlikely to cause myocarditis via cardiac muscle cells. Meanwhile, the researchers detected only a small fraction of spike protein in the cardiac muscle cells of the mRNA vaccine patient and no obvious signs of TLR4. Besides directly damaging the heart muscle cells, the spike protein itself is very inflammatory and may cause systemic inflammation that indirectly causes heart problems,” noted Dr. “That means once the heart is infected with SARS-CoV-2, it will activate TLR4 signaling. Whereas both the spike protein and the TLR4 protein were detected in cardiac muscle cells and other cell types in the COVID-19 patient, neither protein was detected in the healthy heart. Myocarditis occurs when the heart muscle becomes inflamed. The researchers next examined heart biopsies from a deceased patient with COVID-19-associated myocarditis, a patient who died of mRNA-vaccine-associated myocarditis, and a healthy heart. In vitro experiments with rat cardiac muscle cells also led to hypertrophic remodeling and increased levels of inflammatory markers. They found that the SARS-CoV-2 spike protein, and not the NL63 protein, led to heart dysfunction, hypertrophic remodeling- or in other words, cellular enlargement-and cardiac inflammation.
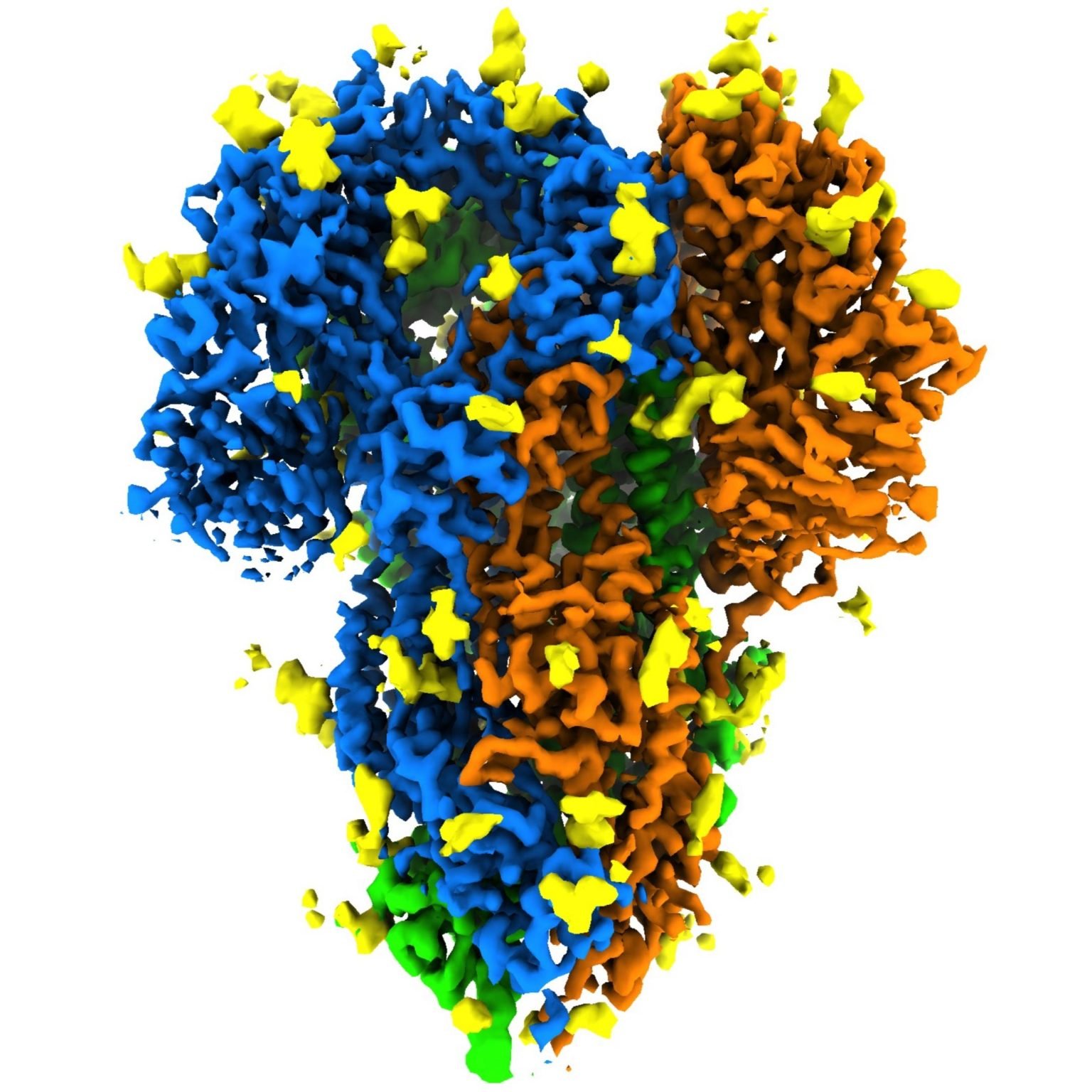
To understand more about how activation of TLR4 signaling may affect the heart, the researchers cloned the SARS-CoV-2 spike protein and the NL63 spike protein, and delivered them to mice via an adeno-associated viral vector. They found that while SARS-CoV-2 activated the TLR4 signaling pathway - a major part of the natural immune response - while HCov-NL63 did not. To test their hypothesis, they compared the ability of both viruses to cause cardiac injury. In the present study, the researchers hypothesized that SARS-CoV-2 may damage the heart via immune responses that are independent of ACE2. Activation of the body’s immune response is essential for fighting against virus infection however, this may also impair heart muscle cell function and even lead to cell death and heart failure,” explained Dr.

“Host natural immunity is the first line of defense against pathogen invasion, and heart muscle cells have their own natural immune machinery. While it causes moderate respiratory symptoms, it does not lead to cardiac injury. HCoV-NL63 is also a coronavirus that enters cells by attaching to ACE2 receptors. The spike protein works by latching onto receptors known as angiotensin-converting enzyme 2 (ACE2) on healthy cells, so it may then enter them. SARS-CoV-2 enters healthy cells via its spike protein, located on its surface. The researchers presented their findings at the American Heart Association’s Basic Cardiovascular Sciences Scientific Sessions 2022. That’s why it’s important to get vaccinated and prevent this disease,” he added. “Our data show that the spike protein from SARS-CoV-2 causes heart muscle damage. Zhiqiang Lin, lead author of the study and an assistant professor at the Masonic Medical Research Institute in Utica, New York. What we suspect is that the spike protein has unknown pathological roles,” said Dr. “It’s already known from the clinical side that COVID-19 infection can induce heart injury, however, what we don’t know is the mechanistic details of how this occurs.
Spike protein covid vaccine series#
Recently, researchers conducted a series of experiments that suggested SARS-CoV-2’s spike protein can lead to heart muscle injury through an inflammatory process. Knowing more about how SARS-CoV-2 affects the heart could help develop new treatments to protect cardiac health. Other research shows that individuals who have contracted COVID-19- even if they were not hospitalized- are at an increased risk of cardiovascular conditions. Studies show that up to 62% of patients hospitalized with COVID-19 experience cardiac injury.


 0 kommentar(er)
0 kommentar(er)
